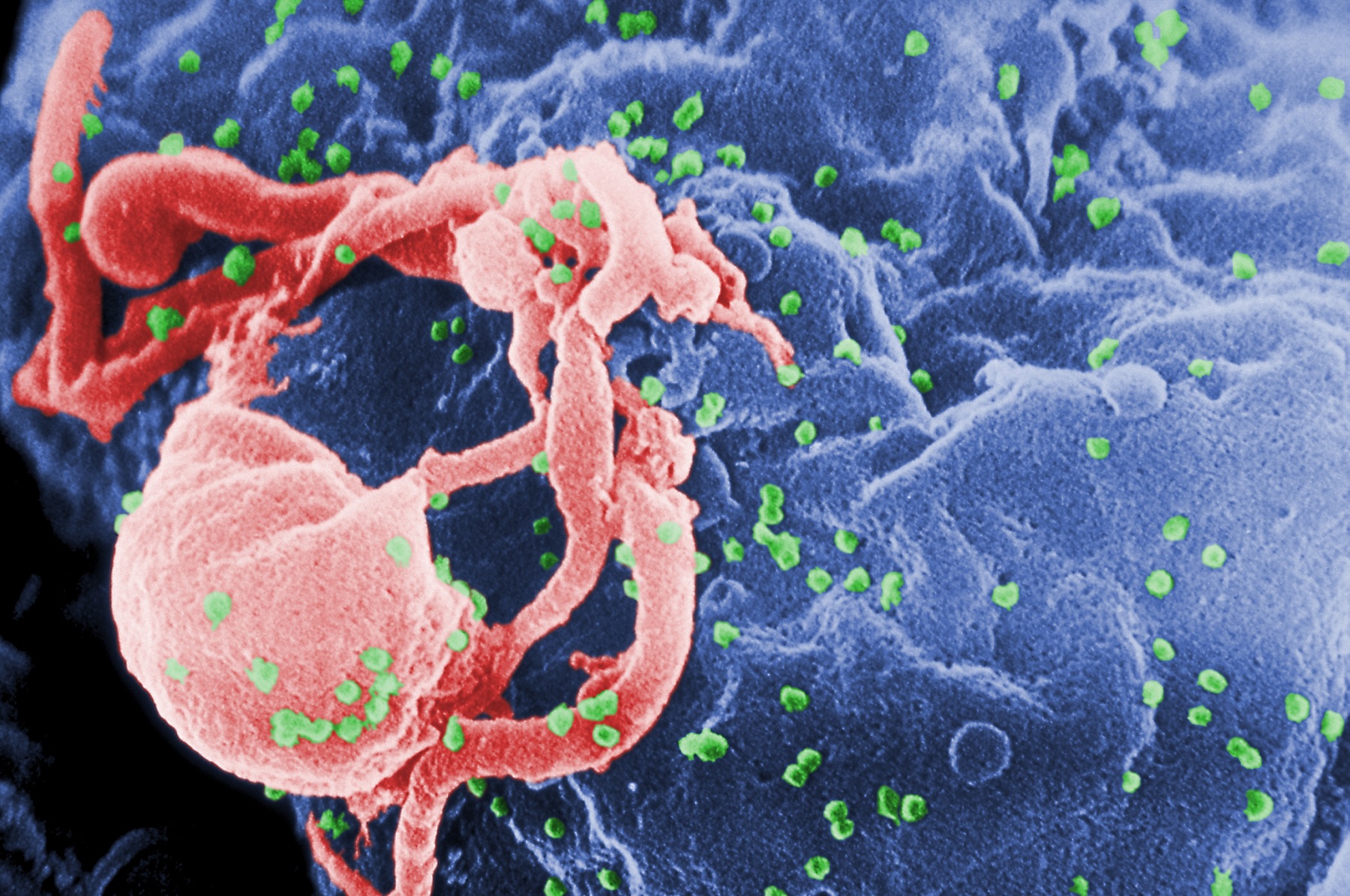
Is COVID-19 riskier for HIV-positive people?
Dr Michael Brady, Medical Director at Terrence Higgins Trust and HIV clinician, offers expert advice.
By Will Stroude
It’s time to separate fact from fiction when it comes to COVID-19 and HIV.
At Terrence Higgins Trust we’re already seeing a big surge in inquiries to our THT Direct helpline from anxious callers about this and I’m grateful to Attitude for the opportunity to discuss the issues, clarify a few things and hopefully reach as many people as possible who might have concerns.
The first thing to say is that there’s no evidence that people living with HIV are at any greater risk of catching coronavirus. Everyone should now be following the government’s advice and doing everything they can to slow the spread of COVID-19; including staying at home, not socialising face-to-face and stopping all unnecessary travel.
COVID-19 infection is likely to be worse in those with a weakened immune system, but this does not mean that all people living with HIV are at increased risk.
Those on HIV treatment with a good CD4 count and an undetectable viral are not considered to have weakened immune systems. Someone’s CD4 count – or white T-cell count – is a measure of how healthy someone’s immune system is.

A ‘good’ CD4 count means anything over 200. But if someone’s CD4 count is less than 200, if they’re not on treatment or if they have a detectable viral load, then it’s particularly important that they follow the advice about how to reduce the risk of catching the virus.
Public Health England has now identified around 1.5 million people who are extremely vulnerable to COVID-19. This includes those who’ve had an organ transplant, people with some cancers or undergoing cancer treatment and those with severe chest conditions such as cystic fibrosis.
They are being advised to ‘shield’ themselves from the virus, which means staying at home at all times and avoiding face-to-face contact for at least 12 weeks (although this time may change). Although people living with HIV are not included in this list, the British HIV Association is advising that those with a CD4 count less than 50 or those diagnosed with an opportunistic infection (a serious illness due to having a weakened immune system) in the last six months should also follow this advice.
Effective treatment means that the vast majority of people living with HIV have an undetectable viral and a good CD4 count. As I said before, the CD4 count s how we measure the health of the immune system. We usually don’t do the CD4 count test anymore because we know that, as long as someone remains undetectable, their CD4 count won’t fall.
That means it could be a number of years since the last time the CD4 count was checked. Our advice is that people shouldn’t worry about this: they don’t need to have a CD4 count repeated now. As long as the viral load remains undetectable, the CD4 count will be as good as it was when it was last tested – and probably better.
What is certainly affecting everyone living with HIV is the fact that HIV clinics are reducing or stopping their face-to-face appointments. This is to reduce the risk of COVID-19 infection and to support people to stay at home as well as freeing up time
for doctors and nurses to be redeployed into hospitals if they are needed to support the extra workload on the NHS.
Rest assured that our priority is, and will always be, people’s health.
Everyone should be aware that we will have to do things differently over the coming months though when it comes to healthcare. For HIV, different clinics may take slightly different approaches but, for the time being routine appointments will be stopped and clinics will only be seeing urgent or emergency cases.

Dr Michael Brady is an HIV clinician and Medical Director at Terrence Higgins Trust
If someone’s well and has an undetectable viral load, we’ll do blood tests less frequently but will always ensure that they have enough medication. There’s no need to stockpile medication – in fact this could put unnecessary strain on the system. We have no concerns about the supply of medication, so the advice is to ensure you always have at least a month’s worth of medication at home.
I hope that’s helpful and reassuring, but if you have any additional questions about COVID-19 in relation to HIV or your sexual health, please contact our helpline THT Direct for free and in confidence on 0808 802 1221 or via the Terrence Higgins Trust website.
We’ll also be issuing guidance on hooking up during the lockdown, ensuring you maintain good sexual health and stopping and then restarting PrEP, as well as any other important health information that’s needed during these strange and challenging times.